When a frail 8-year-old girl’s pneumonia became a dangerous infection, Benjamin Olsson (’99) — a pediatric critical care physician at Medical City Children’s Hospital in Dallas — began treatment in the middle of the night, after her long day of surgery. But she began having seizures, and a blood clot in her brain caused a stroke.
Medical videos and research
Her lungs were severely injured, so Olsson quickly placed her on a ventilator. He then walked into the waiting room to break the news to the parents. And as the little girl’s dad, an NFL lineman more than 6 feet tall and 300 pounds, slept in the small waiting room chair by his daughter’s bed night after night, Olsson’s dedication to the girl only grew.
“Using my skills to save children’s lives is great,” he says. “But it also is important that I’m bedside talking to families when their child is sick or even dying. I want to care for the entire family.”
Olsson and other UNT alumni are some of the best trained physicians, researchers and health educators around because of the solid start in science and research they got at UNT. Some use their comprehensive undergraduate educations to go on to the finest medical and graduate schools in the country.
For others, UNT is the destination for research. They are drawn by state-of-the-art facilities and lab spaces that encourage interdisciplinary and collaborative study. And they are eager to work alongside world-renowned faculty researchers developing software to improve colonoscopies, using light for diagnosis of oral cancer tissues, putting nanophotonics to use for bone repair and drug delivery, exploring plant signaling mechanisms in search of cancer treatments and developing techniques to prevent noise-induced hearing loss from music overexposure.
These UNT experiences inspire students who in turn use their talents to discover new therapies or raise awareness about diseases that plague the world. As compassionate mentors, educators and volunteers, these alumni play important roles in their communities and in individual lives.
In the lab
Edward Ramos’ (’97) first lab was his small family farm in South Texas, where he raised poultry and pigs and observed nature. He was intrigued by the natural order of genetics in plants and animals.
“I was interested in how and why they develop,” he says.
Ramos, whose mother emigrated to the U.S. from Mexico before he was born, studied biology at UNT. His curiosity for nature was fostered by the Ronald E. McNair Post-Baccalaureate Achievement Program, which offers undergraduates firsthand research experience and encourages first-generation or underrepresented students to prepare for doctoral study.
“I applied to UNT because I knew it was a place where I could do real research,” he says.
Ramos earned a master’s degree in biochemistry, microbiology and molecular biology and a doctorate in genetics from Penn State. He continued on to Johns Hopkins for a National Research Service Award postdoctoral fellowship studying the role of insulator proteins in higher-order chromatin organization, which may help treat diseases such as cancer, Parkinson’s disease and diabetes.
“The hallmark of a cancer cell is a bizarre organization of chromosomes, a big black box we don’t understand,” he says. “I’m interested in how genes turn on and off, and what controls that regulation.”
At Johns Hopkins, he also discovered the impact of his own experiences on other ethnic minority students.
“I was approached by some Hispanic undergraduates who felt out of place and were looking for help with real-life experiences so they could assimilate into graduate school,” he says.
This led him to co-found MInDS (Mentoring to Inspire Diversity in Science), an organization dedicated to the recruitment and retention of minorities and women in science. He also co-coordinated a program aimed at exposing high school students to biological research.
Now a postdoctoral fellow at Emory University, Ramos mentors inner-city school children in Atlanta, bringing them to his lab to learn about research inspired by his own work.
“It makes me happy to expose kids to the lab and my research,” he says. “We still don’t have a cure for cancer, but during the last 10 years, we’ve made progress with drug discoveries to slow the disease down. We’re moving in the right direction.”
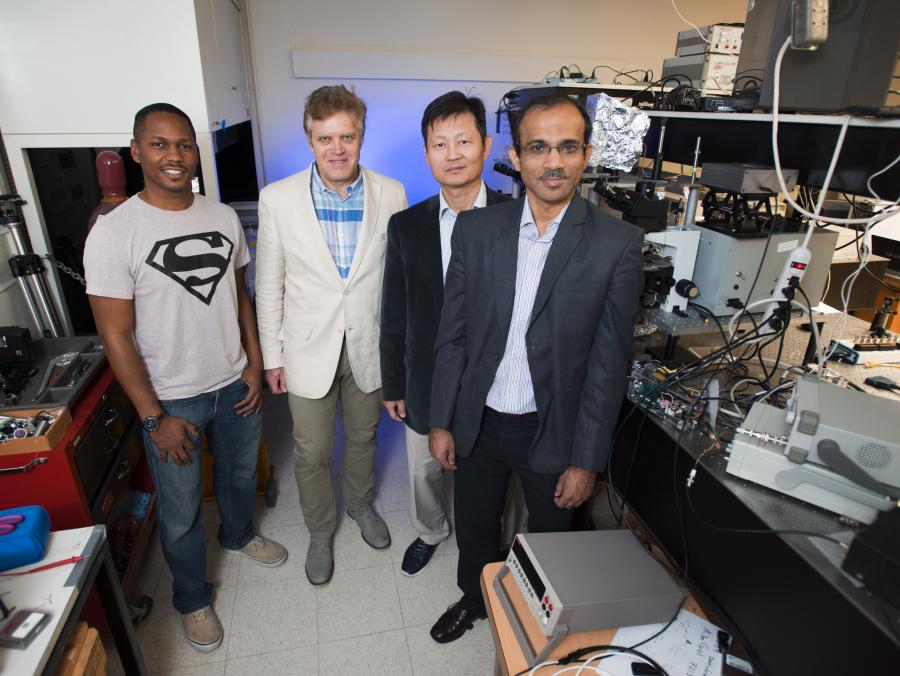
At UNT, investments in collaborative, multidisciplinary research clusters also are leading the way to new discoveries that may help solve some of the largest medical problems of our time.
Members of the Developmental Integrative Biology cluster are using the new state-of-the-art Life Sciences Complex for research in developmental physiology, genomics and the interactions of genes and their environment. Pudur Jagadeeswaran, a professor of biological sciences using zebrafish as a model for prostate cancer research, is one of the first researchers in the country to use the fish to model human disease. His lab — one of the largest zebrafish facilities in the nation — offers valuable learning opportunities for students.
“Zebrafish also are an ideal model to use in studying various types of blood diseases,” says Seongcheol Kim, a research assistant professor who came from Korea to study and work with “Dr. Jag.”
“He is my mentor, not just my employer,” Kim says.

A good experiment
Sharon Y.R. Dent (’80) also has spent her career trying to uncover the mystery of cancer cells, teaching other researchers along the way.
She was a biochemistry undergraduate who knew that she wanted to teach science. But she discovered the excitement of research while learning how to spot her first paper chromatogram, identifying substances of compounds in her campus job as a lab tech assistant.
“It took me hours to do, but I loved every minute of it,” she says. “It was a turning point for me.”
Dent was a member of the Honors Program, which she says helped her develop camaraderie with other like-minded students and introduced her to a broad education.
“When I first started at UNT, I didn’t know what graduate school was,” she says. “But working in the lab opened my eyes to the possibilities.”
Dent earned a doctoral degree from Rice University, and today, is a professor and J. Ralph Meadows Chair of the Department of Molecular Carcinogenesis and director of the Center of Cancer at the University of Texas M.D. Anderson Cancer Center Science Park at Smithville.
The Dent Laboratory, under her supervision since 1993, is making strides in cancer research, examining the role of chromatin and chromatin-modifying proteins in regulating cellular processes. She says that every cell has the same blueprint, the DNA genome, but different cells read it differently.
“We’re helping to better understand how cancer develops and providing new avenues for different therapies,” she says. “But one of the best parts of my job is the science. I love a good experiment.”
At UNT, getting students excited about research includes providing them with opportunities for exchange. David Chi, a student in UNT’s Texas Academy of Mathematics and Science — an accelerated residential program for gifted teens who complete their first two years of college while earning their high school diplomas — aspires to be a physician.
In November, he presented his research on health care barriers faced by the Dallas-Fort Worth homeless population at the North American Primary Care Research Group conference in Banff, Alberta.
“I’ve had the incredible opportunity to work with students and faculty alike in an interdisciplinary manner,” says Chi, president of TAMS’ medical society. “It’s exciting to be able to share my ideas with professionals in a field I am very passionate about.”

A bug for bugs
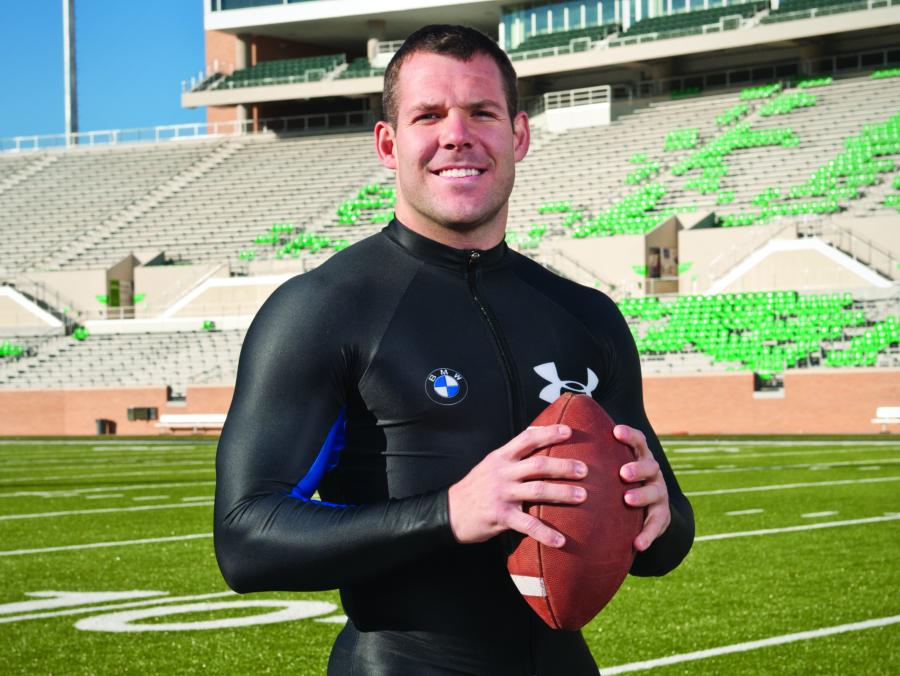
Michael Kavanaugh (’05, ’08 M.S.), a medical entomologist in the U.S. Navy, worked in Jim Kennedy’s biological sciences lab at UNT as an undergraduate. There, he got the bug for bugs.
A disease vector specialist now engaged in world health education and protecting military personnel from infectious diseases, Kavanaugh was a McNair Scholar at UNT, where he developed an interest in vertebrates and published research about storm drains that influence mosquito densities and potential human exposure to arboviruses.
“As an undergraduate, I was given master’s level research and opportunities to lead projects and present at national symposiums,” he says.
After earning his master’s in biology and serving in Afghanistan, Kavanaugh began volunteering for Continuing Promise 2010, a group of military and civilian volunteers who bring medical and engineering services to communities that need it most. He’s worked in South and Central America providing medical treatment, education and public health services.
“I study a wide range of disease-carrying insects, pests that can infest facilities and ships, and provide guidance on proper pesticide use,” he says.
He’s also helping to protect national security by monitoring against vector-borne diseases entering the continental United States.
“By instituting control strategies,” he says, “we prevent populations from large outbreaks of disease.”
Grassroots education
While UNT’s alumni are making important global medical impacts, they also are affecting the daily lives of people in their own communities.
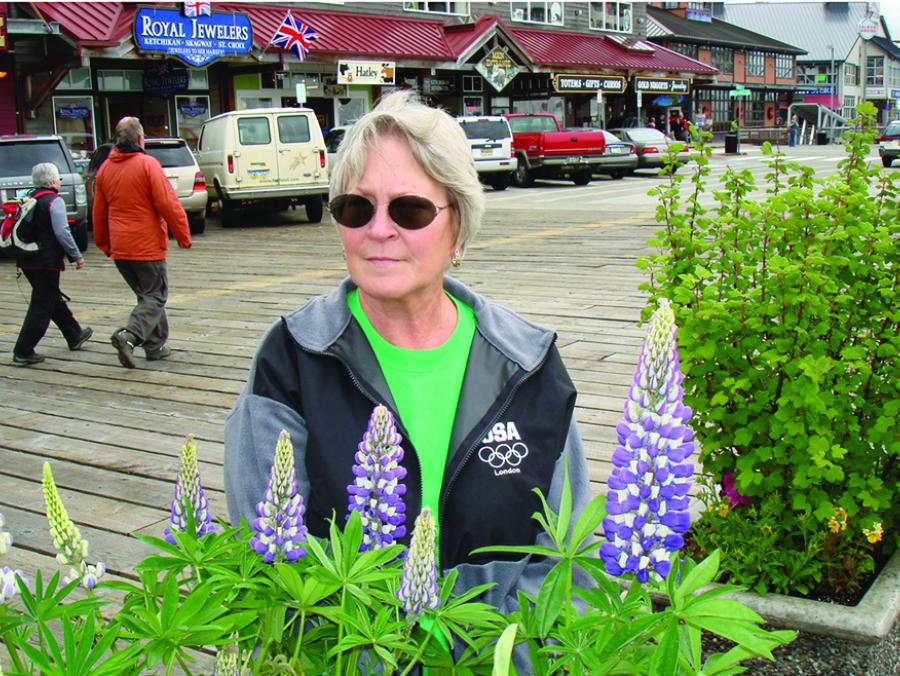
Elizabeth Wagner Carter (’74), who was elected president of the JPS Health Network staff in Fort Worth, holds a faculty position in JPS’ Department of Family Medicine, training future family practice physicians. Carter also oversees physician quality and quality improvement programs.
“Learning how to better prevent falls and infections is proactive, ground-changing behavior for physicians,” says Carter, who also sees patients and specializes in acupuncture and geriatrics.
Her major in social work laid the groundwork for her career as a physician. Carter spent some time as a field social worker for child welfare and nursing homes before attending medical school at the University of Texas Medical Branch in Galveston.
“In addition to learning good interviewing skills and how to connect with people, I have an understanding of real poverty and social issues,” she says.
This perspective guides Carter in community projects on colon cancer and diabetes screening. As the lead for collaborative work through the state of Texas and the UNT Health Science Center’s Community Health Worker Program, she’s educating at the grassroots level about diabetes.
“By going into churches, recreation centers, schools and homes, we’re able to help teach people how to change behaviors to prevent and minimize the disease,” she says. “These are real outcomes.”

Community care
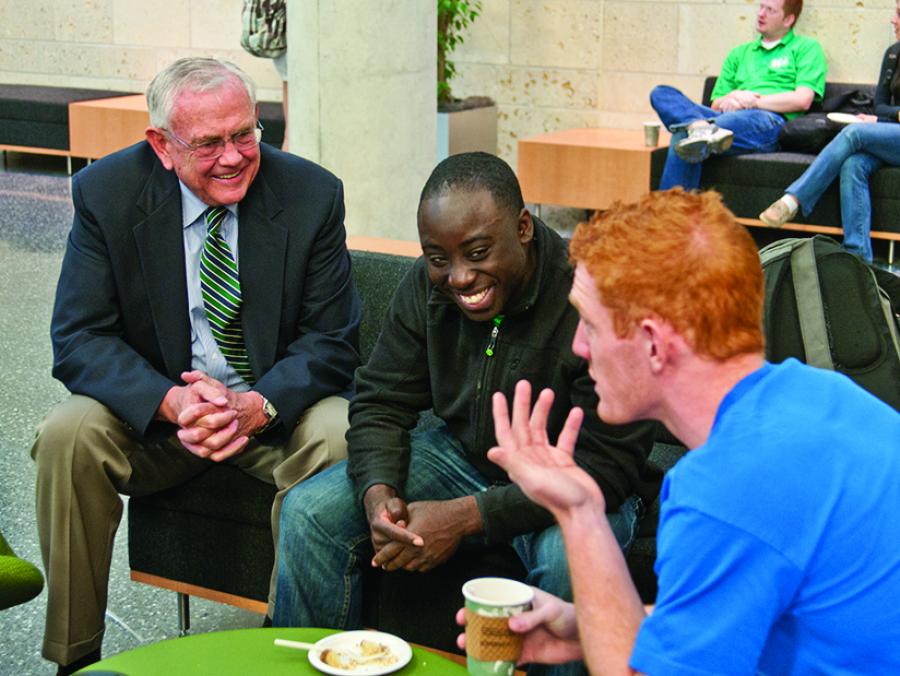
In 1992, Bridgeport’s community hospital closed after serving the Wise County community for more than 50 years. But in 2008, Shawn White (’90), a family physician, and Steven Longacre (’92), an emergency care physician, pooled their medical expertise with 10 other physicians to open North Texas Community Hospital there. The nonprofit community hospital serves the general medical and surgical needs of the county.
The two doctors, friends since high school, now run the 52-bed hospital with services ranging from diagnostic care, physical rehabilitation and women’s health to surgical and emergency care.
“After I had a rough first semester of college, Steve was responsible for reinvigorating my scholarly endeavors,” White says. “He introduced me to Jean Schaake, the pre-med advisor, and got me involved in Alpha Epsilon Delta, the pre-med honor society, which we became officers of in our senior years. This was key to helping me navigate college and I learned that science was dynamic rather than static.”
While at UNT, White not only studied science with his friend, he also met his wife, Debbie White (’89). She is the hospital’s human resources director.
White attended UT Southwestern Medical School in Dallas and completed a residency at JPS Hospital in Fort Worth. Longacre attended medical school at the UT Health Science Center at San Antonio, completing his residency at Palmetto Richland Hospital in Columbia, S.C.
“UNT absolutely prepared me for medical school and the real world,” Longacre says. “In addition to the curriculum, the pre-med advisory committee primed us with pre-interviews so we knew what to expect.”
He and White come back to campus each year to talk to and inspire current UNT pre-med students. Since opening the hospital in 2008, they have seen more than 200 patients each week.
“In November, I delivered my 1,000th baby in Wise County,” White says. “That little girl is the fifth generation of one of the families I’ve had the privilege to care for.”
Longacre agrees that the need he fulfills for their county is rewarding.
“People in the street say thank you for the care I’ve provided,” he says. “I’m part of a community.”
Circle of life
The community Olsson is a part of is mostly made up of children. He treats kids of all ages suffering from conditions that become life threatening, such as cranial facial deformities, infections, seizures, diseases, drug overdoses and drowning accidents. He discovered his interest in medicine as an undergraduate at UNT.
“I wanted to study music, but I fell in love with my science classes,” says Olsson, who was a member of UNT’s basketball band. “A light switch went on, and I took off. The environment at UNT made it one of the most meaningful times of my life.”
Olsson pursued his interest in the sciences with the help of faculty mentors and worked on a research project in his physiology class growing neurons on glass plates. When suffering from early symptoms of diabetes as a student, he visited the campus Health Center under the care of Daniel Forrer and gained insight into the philosophy of osteopathic medicine.
“I became intrigued with the notion of the body as a whole,” Olsson says, adding that Forrer encouraged him to apply to the UNT Health Science Center’s Texas College of Osteopathic Medicine, which is the only osteopathic medical school in Texas and is ranked as one of the top in the country for primary care.
Olsson discovered a natural fit in pediatrics as he and his wife, Lara Olsson (’98), adopted his niece while he was still in medical school.
He completed his residency at Arkansas Children’s Hospital, followed by a fellowship at Children’s MedicalCenter in Dallas.
He has used his training to focus on care that makes a difference. After three weeks of diligent treatment, Olsson’s stroke patient was taken off of the ventilator and slowly started gaining enough strength to be transferred to a rehabilitation facility. Now, Olsson serves on the board of directors of her father’s foundation to assist families who have children in pediatric intensive care units with severe illness.
“Often we can help turn kids around and see them walk out of here,” he says. “For me, that’s the best part.”